If your child has recently been diagnosed with cancer, we understand the fear and powerlessness you are feeling. We have been where you are now, and we know that you are looking for useful information, but we also know that too much information can be overwhelming.
You have your Patient Passport from CHI at Crumlin – this is your bible throughout treatment. We are not medical experts so please refer to your Patient Passport and your team for medical queries. Instead, we focus on providing some helpful tips, information and links which you may need, as well as emotional support.
You might not want or need all of this now but know that you can come back for more information and advice when different situations arise for your family on this new journey you are on.
Knowing the signs of cancer in children, adolescents and young adults
Childhood cancer encompasses children, adolescents and young adults, up to the age of 24. Ireland is currently reconfiguring its paediatric cancer services so that all children and young people up to the age of 19, who are diagnosed with cancer, will be treated in the new children’s hospital.
There will also be key adolescent and young adult centres around the country, which will cater for young adults up to the age of 24.
On average 328 children, adolescents and young adults (aged 0 – 24 years) are diagnosed with cancer every year in Ireland.
Treatments are harsh and can cause life-long side effects, it is estimated that there are over 6,000 adult survivors of childhood cancer living in Ireland and thankfully, due to improved treatments, this number is growing.
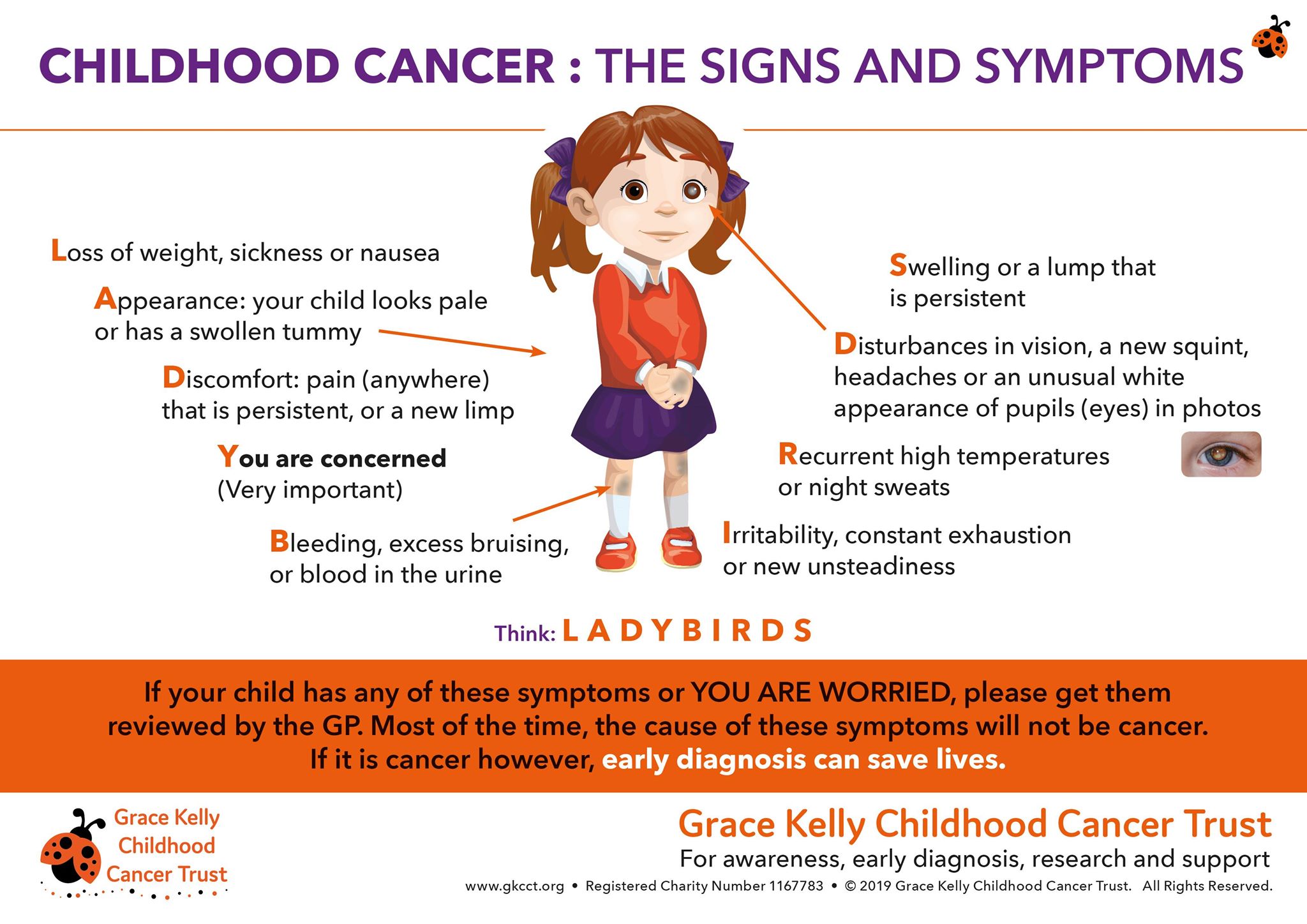
Thank you to the Grace Kelly Trust for this graphic, which outlines the signs and symptoms of childhood cancer. You will find more information at here
Your child’s diagnosis and treatment
Finding out that your child has cancer is overwhelming. Childhood Cancer Ireland is here to support you.
The most common types of childhood cancers include cancers of the blood (leukaemia and lymphoma) primary bone cancers and solid tumours, such as.
Treatment for children’s cancers depends on the type of cancer and can involve chemotherapy, surgery, radiotherapy, targeted therapies, and stem cell and bone marrow transplants.
For more information on your child’s diagnosis and treatment plans please speak with your CNS or Doctor. As Parents we like to understand what we are dealing with, click here is a useful website for information on your child’s diagnosis.
Different things will determine where your child will have their treatment. Usually, it’s to do with their age and the type of cancer they have.
Your child will have needs that require specialised knowledge and skills – not only medical but also psychological and educational. It’s vital that we take into account what is going on in their life – like their education, relationships, emotions, and the role family plays in their life.
CHI at Crumlin
is the National Paediatric Haematology Oncology Centre in Ireland. All children diagnosed with cancer between the age of 0- 16 years here you will meet your child’s specialist team who will manage their cancer treatment as well as the doctors and specialist nurses your child will have access to physiotherapists, occupational therapists, audiologists, dieticians, dentists, pharmacists and psychologists.
Most important to the kids – there is a play specialist available to help them through tough days in hospital.
Your Treatment Outside of Crumlin
As many children live outside the Dublin catchment area, the National Paediatric Haematology/Oncology Programme is supported by 16 shared care paediatric units across Ireland. These shared care hospitals provide essential supportive care and components of treatment locally under the supervision of and in accordance with the National Paediatric Haematology/ Oncology Programme treatment protocols.
Children attending Shared Care Hospitals are treated in isolation rooms, which they cannot leave to use the playroom or other ward facilities. We aim to improve facilities and supports for these children attending the 16 shared care/ regional hospitals, when not required to be in St. John’s Ward.


Life During Treatment
As parents that have walked in your footsteps, here is some useful advice while your child is on treatment:
Welcome to the “NEW NORMAL”
Your child’s whole routine is likely to change during treatment:
- There will be regular hospital appointments, which may involve a lot of travel.
- They may have to stay in hospital overnight for treatment in Crumlin or in one of 16 shared care regional hospitals.
- The treatment may make them feel unwell for a time and may cause changes in their appearance, such as weight loss or hair loss.
Food
Give them a little to eat, but often. Their taste buds will probably be affected, so don’t be surprised if they no longer eat foods that they previously loved. You may also be advised that your child should avoid particular foods entirely while on treatment.
Infections
Keep your child away from sources of infection – such as sick relatives or crowded places. It is important to keep your child away from measles and chickenpox in particular. Pay special attention to dental hygiene and use a soft toothbrush.
If your child is feeling shivery, unwell or running a temperature above 38oC, call St John’s Ward or your local shared care hospital for advice. If in any doubt it is better to call the ward.
Hospital stays
Given the number of hospital visits your child may have during the course of their treatment, it is a good idea to keep a suitcase ready with the essentials, such as pyjamas for both of you, wash bag and favourite games, movies and books that help pass the time in hospital.
While on St. John’s Ward, your child will have access to a Play Specialist and our Beads of Courage Programme, which is open to your child and siblings and can help them better understand their diagnosis and treatment.
School
If your child has to miss school, make plans with teachers so that they can keep up with schoolwork as much as possible when they feel up to it.
Our Lady’s Hospital School, provides for the education of children and adolescents who are attending hospital.
Patients are welcome to continue their education in hospital school and keep up to speed with their studies while you are a hospital in-patient. Their attendance here will be recorded and reported to their own school.
Teaching is available at the bedside for those patients who must stay in the ward.
The Schoolroom is open daily for patients who are mobile and infection-free and whose medical team permit them to attend. The Primary School session is 10 am-12 noon and the afternoon session from 12.50-2.40pm is dedicated to Post Primary Pupils. For more information on Our Lady’s Hospital School please click here.
When your child is able to return to school, give teachers full information about their condition, please ask the principal to send a letter to all parents asking them to advise the school if any family member is affected by measles or chickenpox. If someone is affected your child will need to remain out of school for a period. If you have any difficulties with the school, inform your social worker in Crumlin, who should be able to help. If your child has brothers and sisters, you should also make sure that they have had the MMR vaccine.
Your child’s teacher may be interested in finding out how to support your child so you may like to share the information and resources here.
Webinar: Supporting your child’s transition to secondary
Moving from primary to secondary school is a huge transition for any young person… and their parents! For children who are living with or beyond childhood cancer, who may be dealing with long-term or late effects, this change can be particularly daunting.
This webinar aims to provide information and advice on moving from primary to secondary school, including:
- Applying to secondary school and sharing information.
- Supports available in secondary school.
- Practical tips which may help.
- Dealing with the ‘childhood cancer label’.
Panel:
Lucy Cronly, a parent of a childhood cancer survivor. Lucy has over 30 years’ experience working in social care. Her son underwent treatment for childhood cancer from the age of 11-14 and is now in first year in university. Lucy will share her experiences and advice on communicating with the school to put supports and accommodations in place.
Ger O’Leary, Principal of Celbridge Community School. Ger will talk about the application process, the information communicated from primary to secondary and beginning a dialogue with the school. He will also talk about supports in school that a young person may need to avail of.
Erica McLoughlin, teacher at Our Lady’s Hospital School. Erica works with first year students undergoing treatment on St. John’s ward in CHI at Crumlin and will share her insights into the importance of staying engaged with education and the value of the psychological connection with schooling.
You can watch the webinar below.
Social Activities
Try to keep your child in touch with school pals and other activities. They may miss out on normal social activities and hobbies, depending on their treatment schedule and general health. Tell them they can do all these things when they are feeling better.
Try to arrange some form of activity for them during the day. Playing cards, art, read to them, watch a movie this might help to pass the time. Facetime or write a letter/email friends and family members this will keep them busy too.
Travel costs and practical help
Looking after a sick child can cause unexpected expenses and difficulties. Often parents living outside the Dublin area face the added difficulties of travel and having to organise the care of their families for longer periods while away.
For some there is the added problem of living in an isolated area. Do ask for help from family, friends and neighbours in coping with your new routine. They may be happy to prepare a meal, do a school run, or help with laundry, as they wish to help in a practical way.
Your medical social worker in the hospital will be able to advise you on many of the entitlements that you can apply for. As a first point of call we would recommend that you speak to the social worker who can provide guidance on the supports and grants available to you such as:
- The NCCP Travel 2 Care Grant – administered by ICS
- The Irish Cancer Society’ Children’s fund grant.
- Cliona’s Foundation financial aid grants
- Aiobheann’s Pink Tie financial aid grants
- Gavin Glynn Foundation’s treatment abroad financial assistance grants.
For further information regarding entitlements please see the HSE website
You may have a personal specified critical illness policy, while the last thing you’ll want to think about is your child being critically ill it is worth checking your policy to see of you have the children’s benefit included on your policies.
Depending on the definitions, a payment of between €12,500 and €25,000 might be payable on your child’s cancer diagnosis, which can help with the financial burdens of treatment.


Parents Accommodation & Services
Parents Accommodation in the Hospital St John’s Ward.
Only one parent/ guardian is permitted to stay overnight in St John’s Ward with their child. Patient rooms have either a sleep chair or a window seat that has a dual function as a seat/ bed and a patient wardrobe. There is a kitchen, sitting room toilet and shower facilities available for parents/ guardians on St. John’s Ward.
The patient rooms in the Bone Marrow Transplant Unit (BMT) have a pull down bed for parents/ guardians to sleep. There is a separate kitchen in the Bone Marrow Unit for food preparation for the children in the unit. It also has a washing machine and tumble dryer. This kitchen is for the Bone Marrow Unit only. There is a separate sitting room for parents/ guardians of children in the Bone Marrow Unit. Very specific rules apply to staying with and visiting children on the BMT Unit due to the risks of infection of children on the unit. The nurses there will explain these rules to you.
Complimentary shower facilities are available in the Parents Accommodation Unit on the second floor, for parents who are staying in their child’s room at ward level. Parents/ Guardians must provide their own toiletries and towels. Please speak with the CNM for further information on access.
Second Floor Accommodation
There is single and double room accommodation for up to 44 parents/ guardians on the second floor of the hospital, access is via a stairwell, near the canteen, on the left before the long corridor to St John’s Ward. Bed linen and towels are provided. There are separate bathroom and shower facilities along the corridor. There are 2 sittings rooms and 2 kitchens to prepare snacks. Milk, bread and other basic provisions are supplied. Take Away food is delivered, free of charge, from local outlets such as Dominos Pizza, Subway etc, 7 nights per week. These rooms are available to parents/ guardians only. Children/ siblings of the sick child (unless being breastfed) are NOT allowed access to this unit. The rooms have free Wifi.
Rooms are charged at €18 per night for a single room, €30 per double/ family room. Special rates are available for medical card holders.
Please note that in lieu of Covid-19 and current national guideline restrictions. The Parents Accommodation Unit can only permit one parent/guardian to stay per room.
Other Accommodation
Ronald McDonald Houses:
The Ronald Mc Donald Charity operates two houses. One is on the grounds of the hospital and the other across the road from the hospital at 45 St. Mary’s Drive, Crumlin. The house on the grounds of the hospital has 16 en-suite rooms with TV, laundry facilities (for a small charge) and fully equipped kitchens. Towels and bed linen are provided. The house also has free wifi, a fully equipped playroom, sitting room with library and other relaxation areas. The second House is a smaller building with four en-suite bedrooms and a communal kitchen/ dining and recreation area. It also has a garden and parking. The accommodation is available to families who reside outside the greater Dublin area. There are lengthy waiting lists to access this “home from home” so it’s highly recommended that parents contact the Ronald McDonald team at the earliest opportunity. Volunteers are an integral part of the Ronald McDonald House and most days hot home-cooked meals are provided for the families who reside there.
The charge is €10 per room per night.
To request a room, a family member or guardian must contact the Ronald McDonald House via phone call or email to be placed on the wait list. Please call (01) 4560436 or email [email protected]
A representative of Ronald McDonald House Charities will contact you with room availability.
Unfortunately, due to the nature of the care of the patient, rooms cannot be guaranteed in advance. A family’s length of stay is often uncertain; instead, a family’s name is placed on a wait list for their day of arrival. Rooms are assigned daily as they become available.
www.rmhc.ie
The Louis Fitzgerald Hotel
The hotel The Louis Fitzgerald Hotel offers reduced rate rooms to families attending the hospital of €50 per night (without breakfast).
This must be arranged through Parent Accommodation.
Telephone: 01 4096622.
Car Parking
Car parking on the hospital site is very limited and, between the hours of 9am to 4pm, there is a high demand for car parking spaces.
There is one general patient/visitors car park located at Entrance1 at the Main Outpatients Area on Cooley Road.
All car parks on site are managed on behalf of the hospital by an external contractor.
Please do not park your car on yellow lines or on public footpaths in the surrounding areas of the hospital as clamping is in operation. The hospital encourages the use of public transport where possible.
Concession Rates for Parent/Guardians of Inpatients
The parents/guardians of inpatients who stay more than 10 days at a time, qualify for a reduced car park rate.
Please ask your child’s nurse for an application form. Reduced car park rate is €36 for the first week and €10 per week thereafter.
Disabled Parking Spaces
There are disabled car spaces available directly outside the Main Hospital Entrance and in the patients/visitors Car park. You must display a valid Disable Driver sticker.
Hospital Parking costs (inclusive of VAT)
Parking Payment Machines are only located inside the hospital at Main Reception and inside the foyer of the Main Out Patients Department only – Please note there are no payment machines outside in the car park.
Iveagh Grounds Public Car Park – 10 minutes walk from hospital
Families/ Staff can avail of the public car park in Iveagh Grounds, Crumlin Road, Dublin 12 at a cost of 2euro per day.
This car park is not operated by the hospital and is used by the general public.
Caring for our Super Sibs
Siblings can be deeply affected by their brother or sister’s cancer. This can be an additional worry for parents, at an already difficult time.
As parents we often worry that telling a sibling their brother or sister has cancer will upset them too much. Or that they’re too young to understand. But children are very good at picking up when something ‘big’ is going on. It’s important to talk to them openly and honestly so they don’t imagine the worst.
Children can also feel angry and lose trust if they feel a parent isn’t being truthful with them.
- Talk to your child’s sibling at diagnosis. This may feel very hard but talking and explaining is always better than trying to avoid the subject – even for little children.
- Answer questions as they come up. Be open and honest; this helps your sibling child to trust you.
- Keep siblings up to date if things change. They will also need more detailed information as they get older.
- You don’t always have to communicate things through a conversation. It may be easier for both you and your child’s sibling if you explain things through activity. If they’re little you could try talking to them while playing or reading a story. If they’re a bit older you could talk to them while making a scrapbook, or have a question box. This opens up difficult discussions in an easier way.
Here are some useful aids:
Top Tip
Ask other family members and friends to spend time with the older children in the family. It may be a good idea for one family member or friend to take a special interest in each sibling and attend their school functions, games or help with homework.
Sibling Beads of Courage
Over the last few years, we have worked hard with CHI at Crumlin to introduce a Sibling Beads programme to our existing Beads of Courage programme. The Sibling Beads programme allows siblings to work through their emotions and fears during this difficult time.
Find out more about this programme and how to access it here.
You will find some great advice to support siblings through childhood cancer here.


Partners, family and friends
It can help to share the burden of having a sick child. This can mean working together with your partner, family members or friends to:
Support each other with practical tasks, like going to hospital with your child, minding other children or organising things at home.
Hand in Hand is a National Charity that engage professional services suppliers to provide the following support to all families before, during and after their child’s cancer treatment:
- Support with child care, domestic cleaning services, household laundry and family meals.
- While this can be hard done, share the emotional burden, by talking about feelings together and supporting each other.
- Making sense of the illness. Two heads are better than one when it comes to understanding what the diagnosis and treatment mean.
Try to attend important appointments together, such as meeting the consultant. - Hand in Hand also offer play therapy and counselling services too.
- For more information on their services visit Link to Hand in Hand
Looking after yourself
It can be so difficult to look after yourself when your family is in crisis but it is vital that you take a break and look after your own physical and mental health.
Make a conscious decision to take a mental step back from your sick child from time to time. Take opportunities to spend time by yourself, and with your partner, children, friends, or family.
Get a babysitter occasionally so that you can each pursue your own interests or go out for a few hours.
Ask for help if you need it. Coping with having a child with cancer may bring a couple together. Sometimes, though, the new crisis puts a strain on a relationship. If you feel this is happening, ask for help. Your medical social worker is there to help you during this difficult time.
Seek support from parents groups such as the ICS Peer to Peer Support Service
There are various groups that can offer you, as parents and guardians, extra support. In parent groups you can meet other parents with similar fears and worries. Learn more about services and support for families affected by a children’s cancer diagnosis.
Further and Higher Education
Thankfully, more and more children survive childhood cancer. Anyone who has not lived through a cancer diagnosis and treatment may feel that life returns to normal as soon a treatment has finished. But the life-saving treatments required to save our children and adolescents are toxic and can have long-lasting effects.
In addition, children may have prolonged absences or reduced energy levels that frequently occur during treatment, which may impact their educational progression. Some types of cancer may require therapy to control or prevent spread of the disease to the brain and/or spinal cord (central nervous system).
This therapy can sometimes affect memory and learning abilities. Parents and teachers should be aware of potential educational problems that may be related to cancer treatment so that children and teens at risk can be watched closely and given extra help if the need arises.If your child is looking to go to college, are under 23 years of age and have a disability or diagnosed learning difficulty, they should consider applying for the Disability Access Route to Education (DARE) entry scheme.
Designed to compensate for difficulties posed by studying with a disability, DARE offers successful applicants the opportunity to avail of desired college or university courses that they may not have gotten the points for through the standard application process.
Who can apply for DARE?
You will need to provide evidence of your disability with your DARE application. You can find out what you will need to submit as evidence on the DARE website.
To learn more about DARE visit accesscollege.ie/dare
Webinar on the transition to third level
Moving from second to third level can be daunting for any student and parent, and it is even more so for childhood cancer survivors or adolescents and young adults who are undergoing treatment. No young person affected by childhood cancer is left unmarked by their journey and the treatments needed to save their lives. Many of our adolescents and young adults are dealing with long term and late effects, which may be physical, emotional or cognitive.
This webinar provided information and advice on moving through the senior cycle and moving onto higher and further education. We also looked at DARE (Disability Access Route to Education) and how it applies to young people affected by childhood cancer.
You can watch the webinar below.
Support groups and other useful contacts
The Irish Cancer Society (Services for children with cancer | Irish Cancer Society) has some useful publications for parents, which you may find helpful, as well as further information on the services it offers to children with cancer
Here you will find a list of useful organisations that you may find helpful.